Why Pharmacy-Level Recall Notifications Matter
When a drug gets recalled, it’s not just a paperwork issue-it’s a matter of patient safety. A single contaminated pill or mislabeled bottle can cause serious harm, especially for elderly patients or those on multiple medications. Pharmacies are on the front line: they’re the last point before a drug reaches a patient’s hands. That’s why getting recall notifications fast-and acting on them correctly-isn’t optional. It’s required by law.
The FDA classifies recalls into three levels. Class I is the most serious: the drug could cause serious injury or death. These need to be handled within 24 hours. Class II means the drug might cause temporary health problems or a low risk of serious harm. Class III is the least urgent-usually labeling or packaging errors that don’t affect safety. But here’s the catch: pharmacy-level recall notifications don’t always come clearly labeled. You can’t just wait for an email and assume you’re covered.
Where Recall Notifications Actually Come From
Many pharmacists think they’ll get a recall notice from the FDA website or a public alert. That’s not how it works in real life. The real notification system is layered, and if you’re relying on just one source, you’re at risk.
- FDA MedWatch: Free email alerts you can sign up for at fda.gov/Safety/MedWatch. These go out when the FDA issues a public recall, but they’re often delayed by 6-12 hours. Don’t depend on this alone.
- Wholesaler alerts: Your main distributor-like McKesson, Cardinal Health, or AmerisourceBergen-sends direct notices. Most independent pharmacies get these automatically if they’re under contract. These are usually faster than FDA alerts and include lot numbers and NDC codes. But they’re not perfect: about 1 in 5 alerts are false positives because of mismatched batch codes.
- Pharmacy management systems: Systems like QS/1, PioneerRx, and FrameworkLTC pull real-time FDA data and cross-check it against your inventory. If you have one of these, it will flag a match automatically. This is the gold standard. Hospitals use these almost universally; only half of community pharmacies do.
- Manufacturer direct notifications: Sometimes the drug maker emails or calls you directly. This happens more with brand-name drugs or high-risk products. Always verify these with official sources before acting.
- FDA Enforcement Reports: Published every Wednesday online. These are official but not real-time. Use them to double-check, not to act.
Here’s what the experts say: “At least three redundant systems are mandatory for Class I recalls.” That’s not a suggestion-it’s a regulatory expectation. If you only use one, you’re violating CMS guidelines.
How to Set Up a Reliable Recall Notification System
Setting up a system isn’t about buying expensive software. It’s about building redundancy. Here’s how to do it right, even on a tight budget.
- Register for FDA MedWatch: Go to fda.gov/Safety/MedWatch and create an account. Select “Drug Recalls” and “Pharmacies” as your notification type. You’ll get an email within minutes of a new recall being posted.
- Confirm your wholesaler’s alert system: Call your distributor’s customer service. Ask: “Do you send automated recall alerts via email or system integration? What format do they come in?” If they don’t, ask to be enrolled. Most offer it for free.
- Use your pharmacy software’s recall module: If you use PioneerRx, QS/1, or similar, turn on the recall feed. It should auto-match NDC and lot numbers. If you don’t have this, consider a standalone service like Recall Index (under $50/month) for small pharmacies.
- Assign a recall point person: Designate one staff member-pharmacist or tech-to check all incoming alerts every morning and after lunch. This person should have access to your inventory database and patient records.
- Print and post critical recall info: Keep a printed copy of your current active recalls on the counter or in the dispensing area. Many recalls are missed because staff are distracted by patients or phone calls.
Don’t wait until a recall happens to set this up. Test your system monthly. Send yourself a fake recall notice and see how long it takes to find the drug in your system. If it takes more than 15 minutes, your process needs work.
Verifying a Recall: The 5-Step Protocol
Once you get a notification, don’t panic. Follow this simple, proven checklist.
- Check the classification: Is it Class I, II, or III? This tells you how fast you need to act. Class I? You have 24 hours to remove the product and notify patients. Class II? You have 72 hours.
- Match the NDC and lot number: Every recall notice includes a National Drug Code (NDC) and lot number. Pull up your inventory system and search for exact matches. Don’t guess. If the lot number is “AB123XYZ,” don’t search for “AB123.” It won’t find it.
- Check patient dispensing records: If you’ve dispensed the drug in the last 6 months, you need to notify those patients. Use your pharmacy software to pull a list of patients who received that NDC and lot number. For Class I recalls, you must notify 100% of them. For Class II, 80% is the minimum.
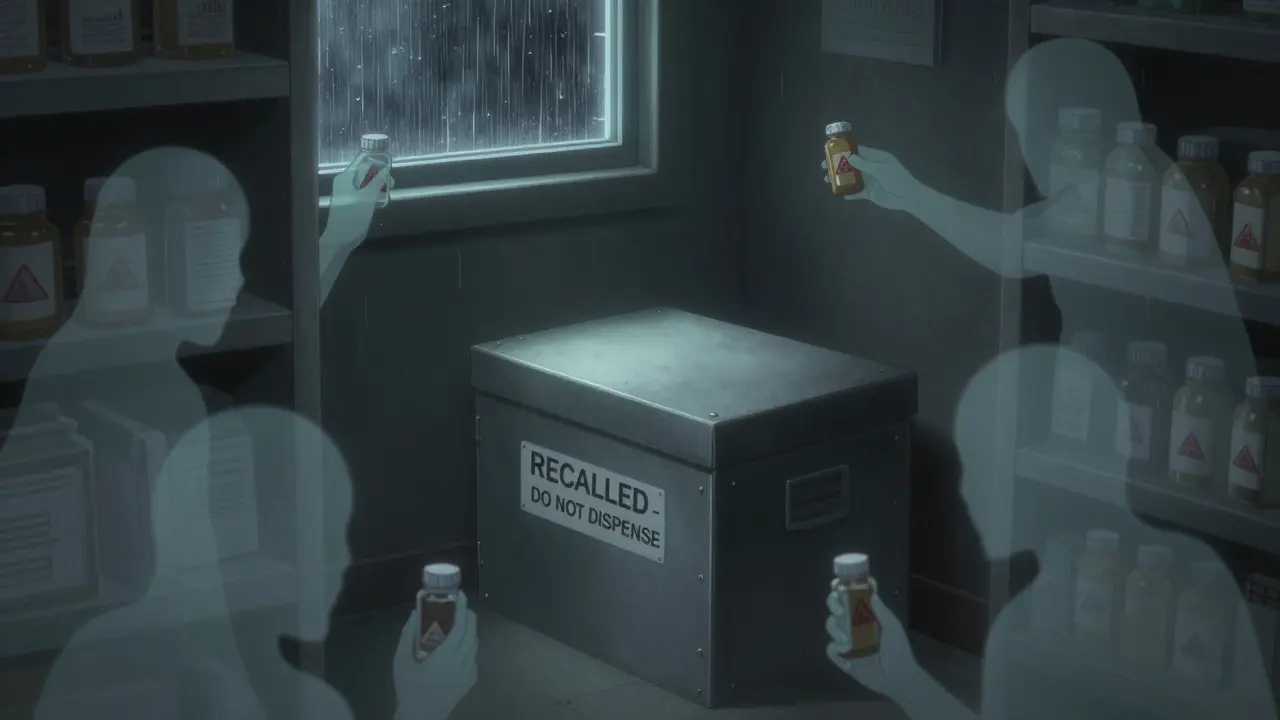
- Remove the product from shelves: Physically pull the drug from inventory. Put it in a locked, labeled box marked “RECALLED-DO NOT DISPENSE.” Do not return it to the wholesaler without written instructions.
- Document everything: Log the date, time, action taken, and who did it. Keep these records for at least three years. The FDA can audit you at any time.
Pro tip: Many pharmacies miss recalls because they don’t check their backstock. Always look in your returns area, storage room, and even the trash can-some techs throw away recalled drugs before they’re officially removed.
Common Mistakes That Lead to Missed Recalls
Even experienced pharmacists make the same mistakes over and over. Here are the top five-and how to avoid them.
- Assuming your system auto-updates: Many pharmacy systems have recall modules, but they’re often turned off or outdated. Check your settings monthly.
- Ignoring email filters: FDA alerts often get caught in spam folders. Add fda.gov and your wholesaler’s domain to your safe sender list.
- Not checking for expired lot numbers: Some recalls only affect batches made before a certain date. If your system doesn’t show expiration dates, manually cross-check.
- Waiting for patient complaints: If a patient calls saying their pill looks different, that’s not a recall-it’s a red flag. Investigate immediately.
- Not training new staff: New techs often don’t know how to respond. Include recall procedures in your onboarding checklist.
A 2023 survey found that 73% of pharmacists had a “near miss” where a recall was received but not acted on because of workflow interruptions. That’s not bad luck-it’s a system failure.
What’s Changing in 2025 and Beyond
The system is getting smarter. By January 2025, all Class I recalls must include patient-level risk data. That means you’ll get not just the drug and lot number, but also which patients are at highest risk based on age, allergies, or other meds.
Blockchain verification is being tested by major players like McKesson and CVS. This will let you scan a pill bottle and instantly see if it’s been recalled-no software needed. But that’s still years away for most small pharmacies.
For now, the biggest change is regulatory: CMS will start requiring pharmacies to prove they can handle recalls during accreditation surveys. If you can’t show a log of your last three recall responses, you could lose your Medicare contract.
What to Do If You Miss a Recall
If you realize you missed a recall, don’t hide it. Act immediately:
- Stop dispensing the drug.
- Notify all patients who received it in the last 6 months.
- Call your wholesaler and the FDA’s MedWatch line at 1-800-FDA-1088.
- Document what happened, why, and how you’ll prevent it next time.
Transparency matters. The FDA rewards pharmacies that self-report and fix problems quickly. They punish those who ignore them.
Final Checklist: Your Daily Recall Routine
Print this. Tape it to your desk.
- ☐ Check FDA MedWatch email every morning
- ☐ Review wholesaler alert inbox
- ☐ Open pharmacy software and run recall report
- ☐ Verify any flagged items against physical inventory
- ☐ Confirm patient notification list is updated
- ☐ Log actions in recall audit trail
- ☐ Train new staff on recall protocol
Spending 10 minutes a day on this could save a life. And it’s the only way to stay compliant.











Lisa McCluskey
January 31, 2026 AT 13:50 PMBeen using the FDA MedWatch + QS/1 combo for years. Works like clockwork. Just make sure your NDC auto-sync is turned on. Saved us during that valsartan mess.
Russ Kelemen
February 2, 2026 AT 07:46 AMThis is one of those posts that makes you realize how much we take safety for granted. The 10-minute daily check isn’t just compliance-it’s ritual. Like brushing your teeth before bed. Skip it once, and you’re gambling with someone’s life. No pressure.
April Allen
February 2, 2026 AT 10:38 AMThe real issue isn’t the tools-it’s the cognitive load. Pharmacists are juggling 12 tasks while a Class I recall pops up. That’s why redundancy isn’t optional: it’s cognitive offloading. If your system doesn’t auto-flag NDC + lot + patient history in one dashboard, you’re running on fumes. And yes, Recall Index is worth the $50. I’ve seen too many small shops get audited because they thought ‘email alerts = covered.’ They didn’t.
Kathleen Riley
February 3, 2026 AT 16:27 PMIt is imperative to underscore that the regulatory expectations delineated herein are not merely aspirational, but constitute binding obligations under Title 21 CFR Part 207 and CMS Conditions of Participation. Noncompliance may precipitate administrative sanctions, including but not limited to revocation of Medicare billing privileges.
Beth Cooper
February 5, 2026 AT 13:43 PMlol the FDA doesn't even know what's in their own database. I got a recall email for a drug that was discontinued in 2018. My wholesaler sent a fake alert because their software glitched. They're all just glorified spam bots. You're better off just calling the manufacturer and asking if they're lying to you.
Donna Fleetwood
February 7, 2026 AT 12:27 PMYou guys are overthinking this. 10 minutes a day. Print the checklist. Tape it to the counter. Done. It’s not about fancy software-it’s about showing up. I’ve worked in 3 pharmacies and every time we did this, no one got hurt. Seriously. Just do the thing.
Melissa Cogswell
February 9, 2026 AT 08:25 AMI just wanted to add-don’t forget the returns bin. Last month, someone tossed a recalled statin into the returns area thinking it was a customer return. We didn’t catch it until the pharmacist went to restock the backroom. Took 4 hours to trace. Now we have a red bin labeled 'RECALLED - DO NOT TOUCH' next to the returns. Small thing. Huge difference.
Diana Dougan
February 10, 2026 AT 21:36 PMWow. 7 steps. A checklist. A point person. You’re all acting like this is brain surgery. I’ve been a tech for 12 years and I’ve never once had a recall hit me while I was on break. Just read the damn email. And if your software can’t auto-flag it, maybe you’re using the wrong one. Also, who prints stuff anymore? 🤡