Infusion Reaction Prevention: How to Stay Safe During IV Treatments
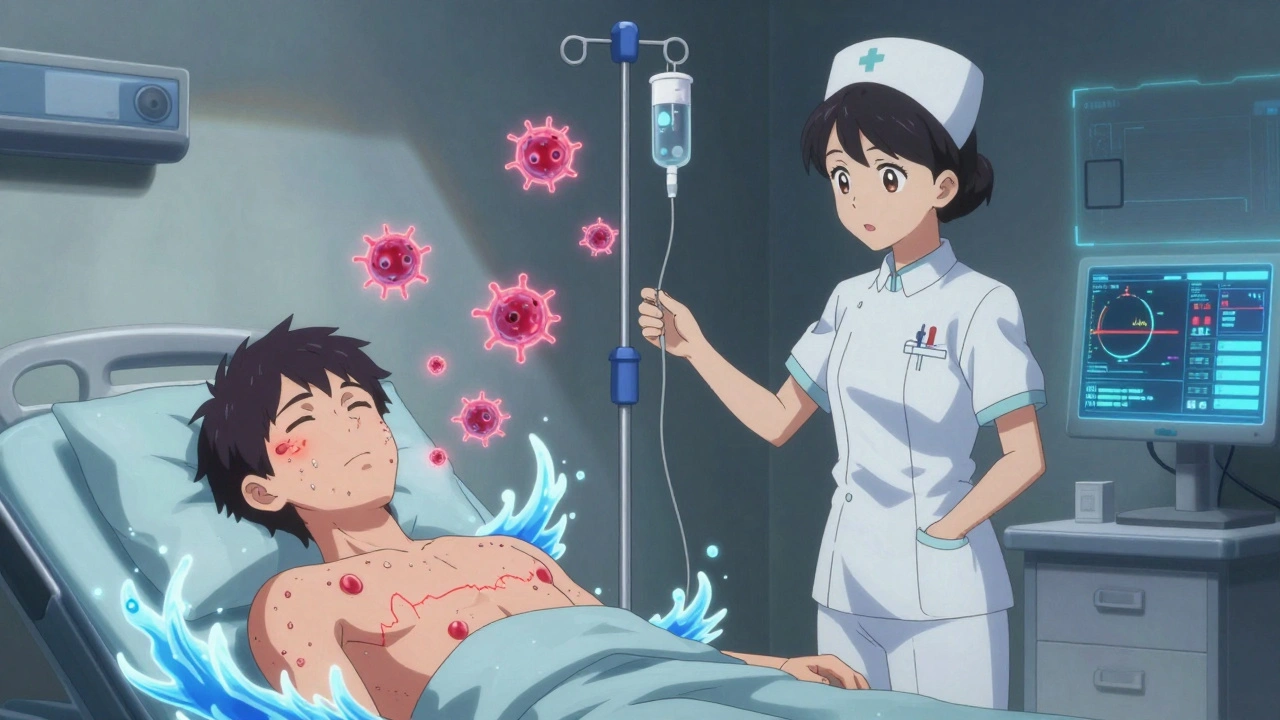
When you get medicine through an IV, you’re trusting your body to handle it quickly and safely. But sometimes, the body reacts—sometimes badly. infusion reaction prevention, the practice of reducing or avoiding harmful responses to intravenous medications. These reactions can range from mild flushing and itching to life-threatening drops in blood pressure or trouble breathing. They’re not rare. In fact, up to 25% of patients on certain infusions like antibiotics, chemotherapy, or biologics experience some form of reaction. Knowing how to spot them early and stop them before they escalate is part of every patient’s safety plan. The key isn’t just avoiding the drug—it’s managing how it’s given, who’s watching, and what your body’s telling you.
IV therapy safety, the system of protocols and monitoring used to protect patients during intravenous drug delivery starts long before the needle goes in. It’s about knowing your history: Do you have allergies to medications? Have you had reactions before? Are you on multiple drugs at once? Even something as simple as the speed of the drip matters. Too fast, and your body doesn’t have time to adjust. Too slow, and the treatment loses effectiveness. Nurses and pharmacists follow strict rules—pre-medication with antihistamines or steroids, slow initial infusion rates, and constant monitoring during the first 15 to 30 minutes. These aren’t just procedures; they’re lifesavers. And if you’ve had a reaction before, you’re not just a patient—you’re someone with a documented risk profile that should be flagged in your records.
allergic reaction to infusions, an immune system overreaction triggered by the drug or its additives doesn’t always mean you’re allergic to the main ingredient. Often, it’s the preservatives, stabilizers, or solvents in the solution—like polysorbate 80 or benzyl alcohol—that set off the response. That’s why switching brands or generic versions can sometimes trigger a reaction you didn’t have before. Your doctor might not even know the difference unless you tell them. Keep a list of every infusion you’ve had and how you felt. Write down the date, the drug name, and what symptoms you had. That record becomes your shield.
Infusion reactions aren’t something you just have to live with. They’re preventable. The best defense is communication: ask questions before the drip starts, speak up if you feel odd, and don’t let anyone rush you. You’re not being difficult—you’re protecting your health. And when you know what to watch for—chills, rash, chest tightness, dizziness—you’re no longer passive. You’re part of the team.
Below, you’ll find real-world advice from patients and providers who’ve dealt with these reactions firsthand. From how to talk to your pharmacist about inactive ingredients to what to do if you react at home after an outpatient infusion, these posts give you the tools to stay in control. No guesswork. No jargon. Just what works.
Biologic Infusion Reactions: How to Prevent and Handle Emergency Situations
Biologic infusion reactions can be scary, but they're preventable and manageable. Learn how premedication, hydration, and emergency protocols can keep you safe on life-changing treatments like infliximab and rituximab.