Pancreatitis – Overview, Causes, and Care
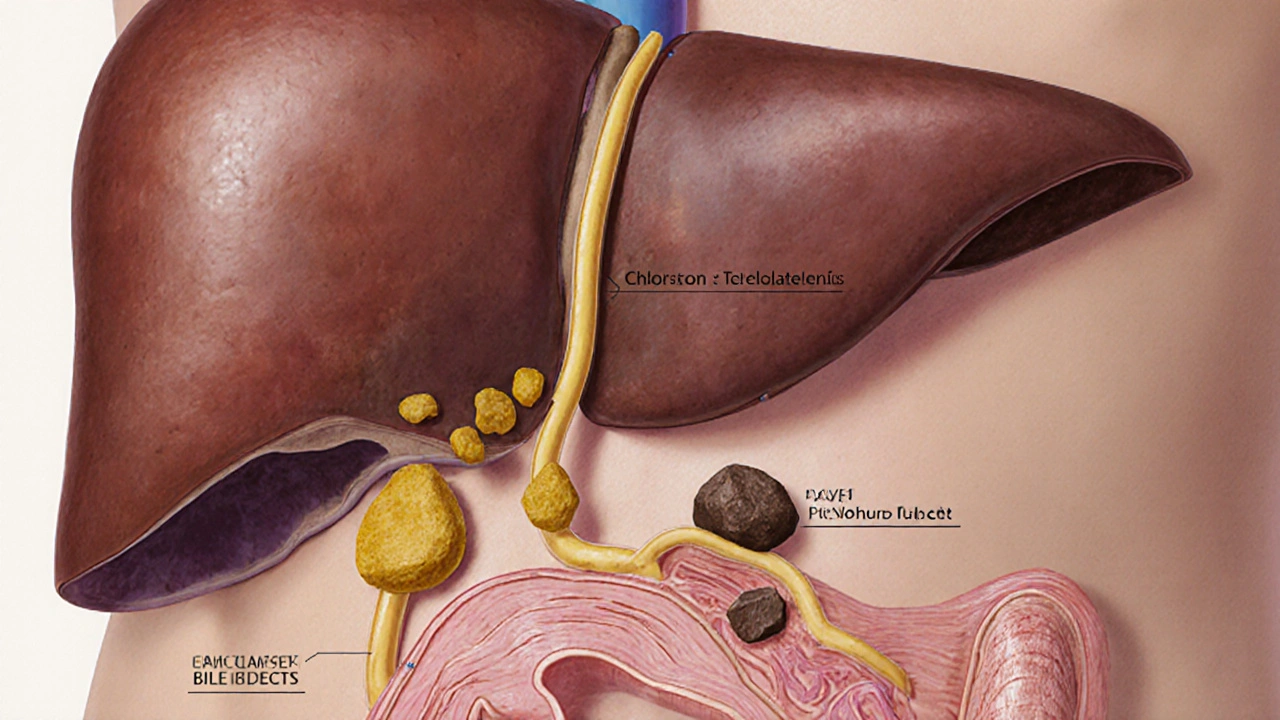
When dealing with pancreatitis, inflammation of the pancreas that can appear suddenly (acute) or develop over years (chronic), the first step is to understand where the problem starts. The pancreas, a gland behind the stomach that produces digestive enzymes and insulin can be attacked by digestive juices, leading to pain, nausea, and long‑term damage. Pancreatitis encompasses both acute and chronic forms, each with its own risk profile. Common triggers include gallstones, solid particles that can block the bile duct and force enzymes back into the pancreas and alcohol abuse, excessive drinking that irritates pancreatic tissue and promotes inflammation. These factors often work together, so a patient with heavy drinking habits and a history of gallstones faces a higher chance of developing chronic pancreatitis. Recognizing the hallmark signs—upper‑abdominal pain that radiates to the back, elevated blood enzymes, and digestive difficulties—helps clinicians act quickly, which can prevent complications like pseudocysts or diabetes.
Managing Symptoms and Preventing Complications
Effective management hinges on eliminating the cause and supporting the organ’s function. If gallstones are the culprit, surgical removal of the stones or the gallbladder is usually recommended; doing so stops the blockage and reduces recurrence. For alcohol‑related cases, complete abstinence is non‑negotiable—continued drinking fuels ongoing damage and worsens outcomes. Nutrition also plays a big role: low‑fat, easily digestible meals ease the pancreas’s workload. When the gland can’t produce enough enzymes, doctors prescribe enzyme replacement therapy, oral pancreatic enzymes taken with meals to aid digestion and nutrient absorption. This therapy directly addresses malabsorption, alleviates steatorrhea, and can improve quality of life. In more severe cases, pain management, endoscopic procedures, or even surgical resection may be necessary, especially when chronic inflammation leads to strictures or calcifications.
Beyond immediate treatment, long‑term monitoring is crucial. Regular imaging checks for structural changes, blood tests for glucose control, and vitamin level assessments help catch secondary issues early. Lifestyle adjustments—maintaining a healthy weight, staying hydrated, and avoiding smoking—complement medical therapy and lower the risk of future flare‑ups. Below you’ll find a curated set of articles that dive deeper into each of these topics, from recognizing early signs to choosing the right enzyme supplement, so you can get the most practical advice for living with pancreatitis.
Gallstones and Pancreatitis: How They’re Linked & What to Do
Learn how gallstones can trigger pancreatitis, spot the symptoms, understand diagnosis and treatment options, and discover prevention tips to avoid future episodes.