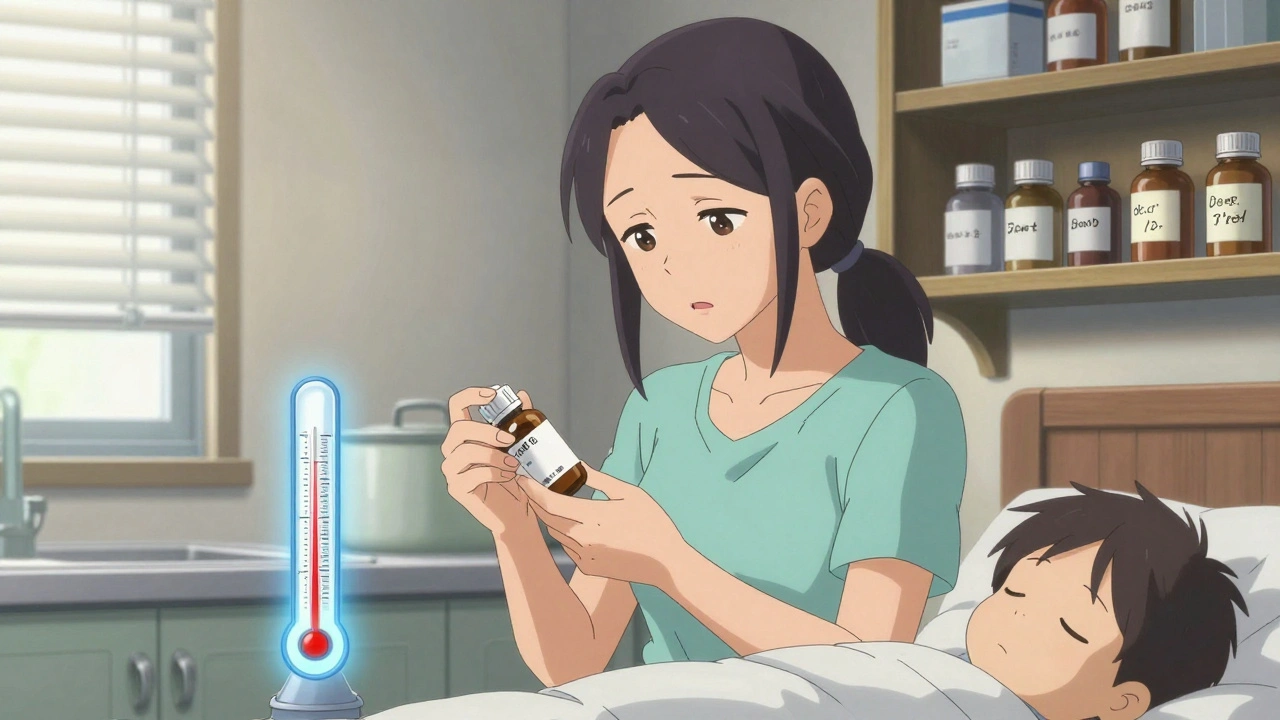
Antibiotic Suspension Storage: How to Keep Your Medicine Safe and Effective
When you pick up an antibiotic suspension, a liquid form of antibiotic designed for easy swallowing, often used for children or people who can’t swallow pills. It’s not just water with medicine—it’s a carefully balanced mix that can break down if stored wrong. Many people assume all medicines are the same: pop the cap, take it, and forget it. But antibiotic suspension storage isn’t optional—it’s critical. If you leave it on the counter when it needs the fridge, or keep it too long after mixing, you might not get the full dose. And that means the infection could come back stronger.
Some suspensions, like amoxicillin or azithromycin, need to be refrigerated after mixing. Others, like cephalexin, are fine at room temperature. But even the room-temp ones have a short window—usually 7 to 14 days after mixing. After that, the active ingredients start to fall apart. You won’t see it. You won’t taste it. But your body will feel the difference. And if you’re giving it to a child, getting the wrong amount can mean the difference between healing and a hospital visit. antibiotic shelf life, how long a mixed antibiotic stays effective after preparation depends on the drug, the preservatives used, and how it’s kept. The label says it all, but most people don’t read it. Pharmacists know this. That’s why they often hand you a little card with storage instructions. Don’t toss it.
refrigerated antibiotics, liquid antibiotics that must be kept cold after mixing to preserve potency are especially tricky. Cold doesn’t mean frozen. Freezing can ruin the suspension’s texture and make it hard to shake properly. And if you forget it’s in the fridge and leave it out overnight? It’s probably still okay—but don’t make a habit of it. Temperature swings are the enemy. Even if the bottle says "store at room temperature," keep it away from sunlight, heat sources, or humid places like the bathroom. Moisture and warmth speed up breakdown. And remember: if it smells funny, looks clumpy, or has changed color, throw it out. No second chances with antibiotics.
Why does this matter so much? Because misuse feeds antibiotic resistance. When you don’t get the full dose, the toughest bacteria survive. They multiply. And next time, the same drug won’t work. This isn’t science fiction—it’s happening right now, in homes, clinics, and hospitals. Proper antibiotic stability, how well a medication maintains its chemical structure and effectiveness over time under specific conditions isn’t just about saving money. It’s about keeping antibiotics effective for everyone.
Below, you’ll find real advice from people who’ve dealt with this—parents who ran out of medicine because they didn’t know how long it lasted, seniors who mixed it wrong, caregivers who thought "it’s still good" because it didn’t expire on the bottle. These aren’t hypotheticals. They’re stories that show why storage isn’t just a detail. It’s part of the treatment.
How to Store Antibiotic Suspensions for Children Properly: A Clear Guide for Parents
Learn how to properly store children's antibiotic suspensions to ensure they work and don't cause resistance. Know which ones need refrigeration, when to throw them out, and how to avoid common mistakes.