Biologic Infusion Reactions: What They Are, How to Spot Them, and What to Do
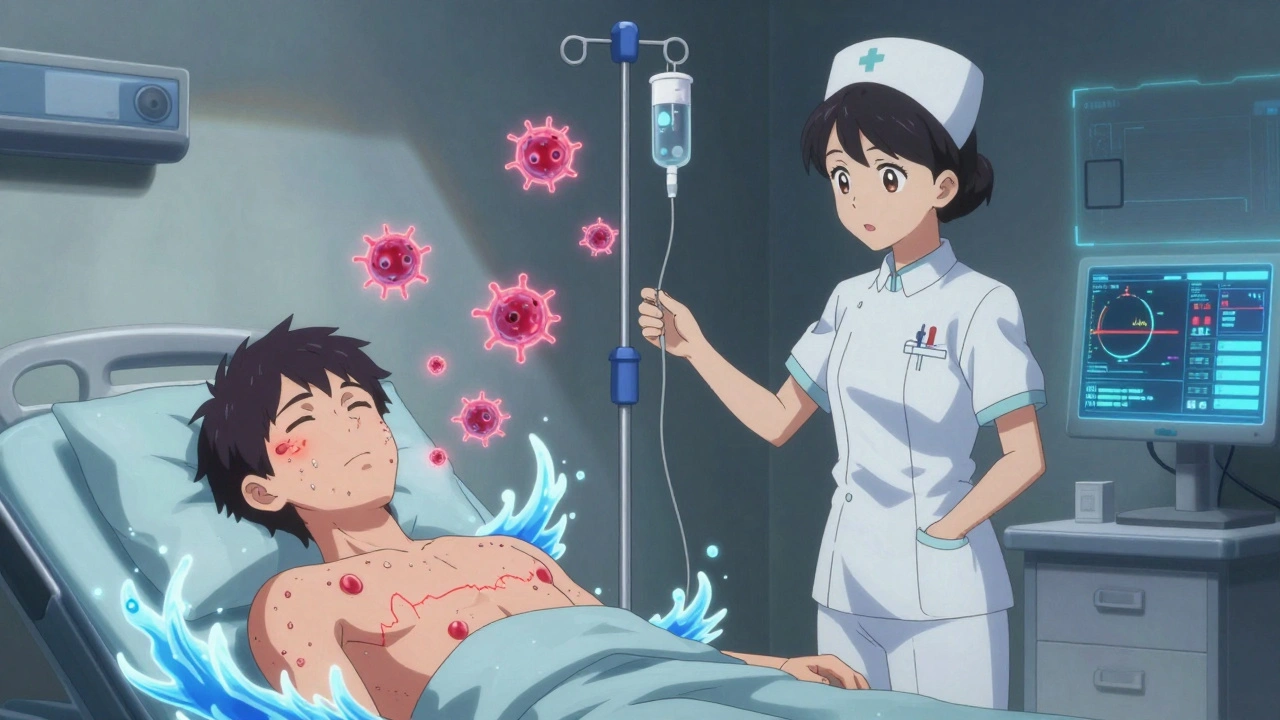
When you get a biologic infusion reaction, an unexpected immune response triggered by biologic drugs given through an IV. Also known as infusion-related reactions, it happens when your body reacts to proteins in the medication—not because of an allergy, but because your immune system sees them as foreign. These reactions don’t mean the drug isn’t working. In fact, they’re often a sign your immune system is active, which is exactly what these drugs are designed to do. But when they get too strong, they can cause chills, fever, nausea, or even trouble breathing—and that’s when you need to act fast.
Biologic infusion reactions are most common with drugs used for autoimmune diseases like rheumatoid arthritis, Crohn’s disease, or psoriasis. They’re also seen with cancer treatments like rituximab or trastuzumab. The reaction usually shows up during the first or second infusion, and it’s more likely if the drug is given too quickly. That’s why most clinics start slow and watch you closely for at least 30 minutes after starting. Biosimilars, drugs designed to copy brand-name biologics with near-identical effects. Also known as follow-on biologics, they carry the same risk of infusion reactions because they work the same way. Even if you’ve taken the original drug without issues, switching to a biosimilar can still trigger a reaction. It’s not because the drug is weaker—it’s because your body doesn’t know the difference.
Some people think these reactions are rare, but they’re not. Studies show up to 30% of patients on certain biologics experience mild to moderate reactions, especially in the first few infusions. The good news? Most are manageable. Slowing down the drip, giving antihistamines or steroids before the infusion, or spacing out treatments can make a big difference. If you’ve had a reaction before, your provider will adjust your plan—maybe start with a lower dose, or add pre-medication. You’re not stuck with the same risk each time.
What you can’t control is how your body responds. But you can control how you speak up. If you feel hot, itchy, or tight in the chest during an infusion, tell the nurse right away. Don’t wait. Don’t assume it’s just nerves. Early action stops mild reactions from becoming emergencies. And if you’ve ever had a reaction, keep a note in your phone or wallet with what happened, when, and what helped. That info saves time and stress next time.
These reactions are tied to how biologics are made—using living cells to create complex proteins. That’s why they’re different from regular pills or even generic drugs. You can’t swap them like you would aspirin. Their structure matters. Their purity matters. Even tiny changes in manufacturing can affect how your body reacts. That’s why the FDA requires strict testing before approving any biologic or biosimilar. But no test can predict how your immune system will respond. That’s why monitoring during infusion isn’t optional—it’s essential.
What you’ll find below are real, practical guides from patients and providers who’ve dealt with this. You’ll learn how to prepare for your next infusion, what symptoms to watch for after you leave the clinic, how to talk to your doctor about switching drugs, and why some people never have a reaction while others do. It’s not about fear. It’s about knowing what’s normal, what’s not, and how to stay in control when your body sends a signal you didn’t expect.
Biologic Infusion Reactions: How to Prevent and Handle Emergency Situations
Biologic infusion reactions can be scary, but they're preventable and manageable. Learn how premedication, hydration, and emergency protocols can keep you safe on life-changing treatments like infliximab and rituximab.