Medication Safety: Protect Yourself from Errors, Interactions, and Side Effects
When it comes to your health, medication safety, the practice of using drugs correctly to avoid harm while maximizing benefit. Also known as drug safety, it’s not just about following labels—it’s about understanding how your body reacts, how pills interact, and how systems fail before they reach you. Every year, hundreds of thousands of people in the U.S. are harmed because someone—pharmacist, doctor, or even the patient—missed a simple step. It’s not always negligence. Sometimes it’s poor communication, outdated systems, or just too many pills on a crowded nightstand.
Medication errors, mistakes in prescribing, dispensing, or taking drugs. Also known as drug mistakes, it can happen at any point—from the hospital to your kitchen table. Using two patient identifiers like name and date of birth isn’t bureaucracy; it’s a lifeline. Barcode scans, EMPI systems, and double-checks exist because a single mix-up can kill. And it’s not just about getting the wrong drug—it’s about the wrong dose, the wrong time, or the wrong person. Seniors on five or more pills? You’re at higher risk. That’s why combination medications that merge multiple drugs into one tablet aren’t just convenient—they’re lifesavers.
Generic drug absorption, how quickly and completely a generic version enters your bloodstream compared to the brand. Also known as bioequivalence, it isn’t a guess. The FDA requires generics to match brand drugs within 80% to 125% absorption. Most do. But if you’re on thyroid meds, blood thinners, or seizure drugs, even small shifts matter. That’s why some people notice a difference—even if science says they shouldn’t. And then there are interactions. Steroids can trigger psychosis. Nortriptyline and alcohol? A dangerous combo. Calcium acetate might affect your eyes. Spicy food and pantoprazole? They team up to wreck your stomach. These aren’t rare cases. They’re documented, predictable, and preventable—if you know what to watch for.
Medication safety isn’t just a hospital rule. It’s your daily responsibility. It’s asking your pharmacist why a new pill looks different. It’s writing down every drug you take—including supplements. It’s recognizing that prednisone can make you weep for no reason, or that statin cramps might be nerve damage, not muscle strain. It’s knowing that a digital therapeutic app can help you stick to your meds—or accidentally interfere with them. And it’s realizing that your body doesn’t care if a drug is cheap or branded. It only cares about what’s in it, how much, and when you took it.
Below, you’ll find real, practical guides written by people who’ve seen the fallout. From how to spot a mupirocin allergy to why triple inhalers for COPD aren’t all the same, these posts cut through the noise. No fluff. No theory. Just what works, what doesn’t, and what you need to ask before you swallow the next pill.
Patient Safety Goals in Medication Dispensing and Pharmacy Practice: What Hospitals Must Do Now
Medication errors cause thousands of preventable deaths each year. Learn the mandatory patient safety goals hospitals must follow, why traditional methods fail, and what real-world solutions are working in 2026.
Addressing Health Disparities in Medication Safety Research
Medication safety disparities disproportionately affect racial minorities, low-income patients, and non-English speakers due to systemic biases, lack of representation in clinical trials, and unequal access to care. Addressing these gaps requires systemic change, not just better training.
How to Check for Pharmacy-Level Recall Notifications: A Step-by-Step Guide for Pharmacists and Staff
Learn how to check for pharmacy-level drug recall notifications using FDA alerts, wholesaler systems, and pharmacy software. Step-by-step guide for pharmacists to avoid missed recalls and ensure patient safety.
Barcode Scanning in Pharmacies: How It Prevents Dispensing Errors
Barcode scanning in pharmacies prevents 1.3 million medication errors annually by verifying the right patient, drug, dose, route, and time. Learn how it works, where it fails, and why it's the gold standard for safety.
Medication Errors vs Drug Side Effects: How to Tell Them Apart and Why It Matters
Learn how to tell the difference between medication errors and drug side effects-why it matters, how to spot each one, and what you can do to stay safe. Real data, real stories, real solutions.
Medication Safety for Caregivers: How to Protect Loved Ones from Dangerous Errors
Learn how caregivers can prevent dangerous medication errors at home. From accurate dosing to pharmacist reviews, these practical steps protect loved ones from harm and hospitalization.
How to Ensure Medication Safety in Hospitals and Clinics
Medication errors harm hundreds of thousands in U.S. hospitals each year-but most are preventable. Learn how hospitals are using best practices, technology, and culture to stop errors before they happen.
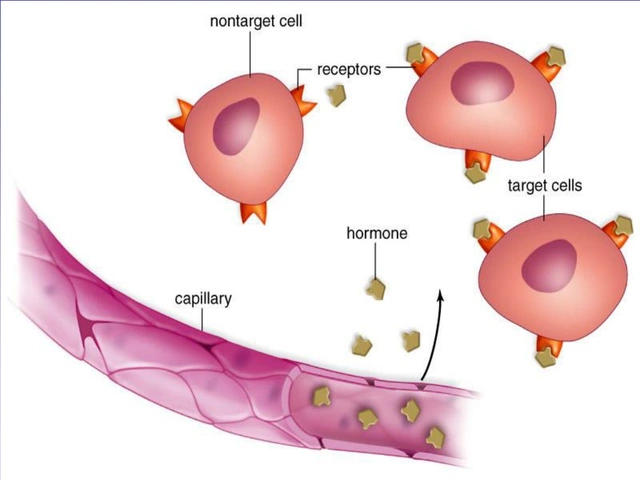
How Medicines Work and When They're Safe to Use
Learn how medicines interact with your body at a molecular level and why understanding their mechanism of action is critical for safe use. Real examples show how knowing how a drug works prevents harm and improves outcomes.
Health Literacy Strategies: Understanding Medication Labels and Dosing
Learn how to read medication labels correctly and avoid dangerous dosing errors using proven health literacy strategies. Simple changes like using morning/noon/evening/bedtime instructions and pictograms can save lives.
Look-Alike, Sound-Alike Medication Names That Cause Errors: Real Risks and How to Stop Them
Look-alike, sound-alike (LASA) drug names cause thousands of medication errors each year, leading to overdoses, hospitalizations, and even deaths. Learn which drugs are most dangerous, why mistakes keep happening, and how to protect yourself.